Skin Check Clinic Brisbane
Skin Cancer Checks
Visit the leading skin check clinic in Brisbane for expert skin cancer checks and mole assessments. Our experienced doctors deliver thorough, professional examinations – giving you confidence, clarity, and proactive advice and treatments recommendations.

Head to Toe Skin Examinations
Full Body Skin Cancer Check
At ISO Clinic, we offer comprehensive skin cancer checks performed by qualified doctors using advanced diagnostic tools. Whether you need a routine full-body exam or have concerns about a specific mole or lesion, our skin cancer clinic in Brisbane is here to provide thorough care and peace of mind. Early detection can save lives – check for skin cancer today with no referral needed.
Why choose ISO Clinic for your skin cancer check?
- Doctor-led care: Every skin check is performed by an experienced GP with additional training in skin cancer detection.
- Advanced diagnostics: We use dermatoscopes and other medical-grade tools to examine your skin thoroughly.
- Histology testing: Suspicious lesions can be biopsied and sent for pathology review.
- Confidential and comfortable: Male and female doctors are available to respect your preferences and privacy.
- Precision technique for minimal scaring: Scarless mole removal can be achieved using Advanced Radiofrequency Technology.
- Convenient Brisbane location: Located in Upper Mount Gravatt, we serve patients from across the Brisbane region.
For peace of mind, we’ve describe the process below. We aim to make the experience as comfortable as possible and your concerns and feedback and questions before, during and after the process is always welcome.
- During the check, we will visually inspect and palpate your skin, and use a dermatoscope to get a closer look at any moles or lesions.
- You will be asked to undress to a level that you are comfortable with, and a modesty sheet is provided for your privacy.
- Typically, we begin by examining one side of your body before moving to the other, starting from the scalp and moving down to the toes.
- For the most accurate examination, we recommend wearing light makeup or none at all, and removing nail polish if you have any moles under your nails.
- We respect your privacy and do not routinely check areas covered by underwear unless you give consent. It’s important to remember that skin cancer can develop on non-sun-exposed areas as well.
After the check, if we identify any lesions of concern, we may take photos for monitoring purposes, or perform a biopsy or excision.
If no suspicious lesions are found, we will advise you on how often you should have skin checks based on your individual risk factors. Thank you for choosing us for your skin checks. We are committed to providing you with the highest level of care.
At ISO Clinic, your skin health is our top priority. Book your skin cancer check today and take a vital step towards safeguarding your health.
Dr. Tina Fang and Dr. Jack Fu are committed to addressing your concerns promptly
Even if you suspect it might be nothing, it’s always best to have it examined. At our clinic, we use Dermatoscopy to provide a thorough assessment, ensuring that even the smallest changes are carefully evaluated.
It’s always better to be safe and have any changes checked by our experts.


Qualifications
Fellowship of the Australasian College of Aesthetic Medicine

Fellowship of the Royal Australian College of General Practitioners 2019

Skin Cancer College Australasia
Advanced Skin Surgery

Master Medicine (Skin Cancer) Candidate
Understanding Melanoma:
Australia's National Cancer
Australia has the highest melanoma rates worldwide, often called ‘Australia’s national cancer.’ It’s crucial to recognise its prevalence and severity because of its potential for early detection and successful treatment. Melanoma can spread to many body parts, commonly affecting the lymph nodes, lungs, liver, bones, and brain. Early detection is key to managing its spread effectively.
Approximately
Australians are diagnosed each year
Around
Australians die annually from melanoma
Most common cancer in Australians aged 20 to 39
Second most common in men, after prostate cancer.
Third most common in women, after breast and colorectal cancer.
Prevention and Detection
Early detection can lead to a 90% cure rate through surgical intervention.
Significant progress has been made in the last decade, with the 5-year survival rate for advanced melanoma increasing from less than 10% to over 50%.
If you notice any changes or new spots on your skin, don’t hesitate to book a quick spot check. Dr. Tina Fang and Dr. Jack Fu are committed to addressing your concerns promptly. Even if you suspect it might be nothing, it’s always best to have it examined.
At our clinic, we use Dermatoscopy to provide a thorough assessment, ensuring that even the smallest changes are carefully evaluated. It’s always better to be safe and have any changes checked by our experts.


How to Check Your Skin
ABCDE Method of Identifying Melanoma
A for Asymmetry – One half of the spot does not match the other.
B for Border – Edges are irregular, ragged, or blurred.
C for Colour – Varies within the same spot.
D for Diameter – Larger than 6mm or growing.
E for Evolving – Any change in size, shape, colour, or symptoms such as itching or bleeding.
If you notice any changes or new spots on your skin, don’t hesitate to book a quick spot check
Types of Pre / Skin Cancers
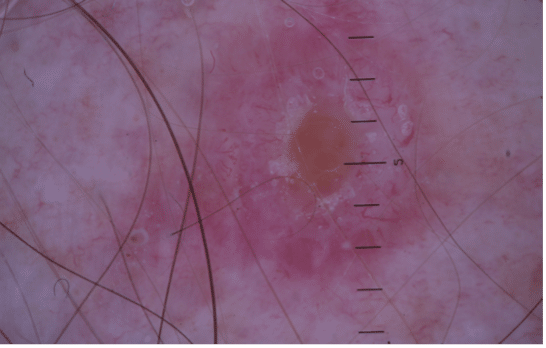
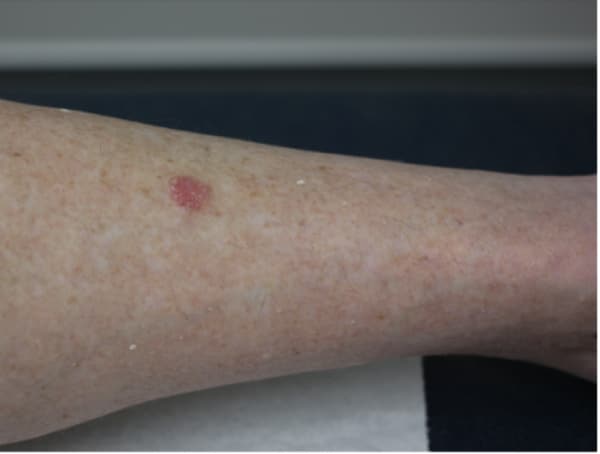
1. Solar Keratosis / Sun Damaged Skin
Solar keratosis, also known as actinic keratosis, is particularly common in Australia due to high UV radiation exposure. These rough, scaly patches on the skin are precursors to squamous cell carcinoma and typically appear in sun-exposed areas like the face and hands.



Treatment Options for Actinic Keratoses
1. Cryotherapy:
Pros: Quick treatment with minimal post-care, suitable for one solitary lesion.
Cons: May require multiple sessions for effectiveness; not suitable for a large field of sun-damaged skin. Risk of hypopigmentation scar.
2. Shave, Curettage, and Electrocautery:
Pros: Immediate removal of the lesion, effective for thick keratoses, suitable for one solitary lesion.
Cons: Some of scarring and requires careful wound care; not suitable for a large field of sun-damaged skin.
3. Topical Treatments:
Two topical cream treatments available.
Pros: Effective at killing precancerous cells. Might be eligible for PBS subsidy. General patient charge $30-35+F17
Cons: Can cause significant skin irritation. Apply to the affected area 2 times a day for 2 to 4 weeks. (Sometimes, not practical). Prolonged treatment duration, may cause local skin reactions.
4. Photodynamic Therapy (PDT):
Pros: Suitable for sun-damaged skin on the face, ears, scalp, and chest; one-day treatment, generally less painful. Downtime of 4-5 days.
Cons: Higher cost compared to other treatments. $600 per region. (Both one side of hands are one region, both one side of forearms is one region). May need 2 treatments depending on your severity.
Prevention of Actinic Keratoses
Apart from practicing sun-smart and attending regular skin checks. (which we are all aware of). Some studies have shown a reduction of Solar Keratosis with:
- Taking Vitamin B3) 500 mg twice.
- Applying prescription Vitamin A.
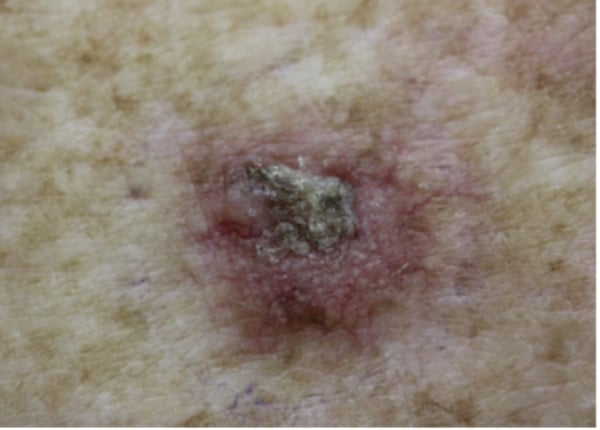
2. Basal Cell Carcinoma (BCC)
Basal Cell Carcinoma (BCC) is the most common form of skin cancer. While BCC is known for its local invasiveness, it rarely metastasises due to its typically slow growth and minimal tendency to spread beyond its original site. However, if left untreated, BCC can cause significant local destruction, potentially eroding through skin and soft tissues to reach underlying bones.
Understanding Basal Cell Carcinoma
BCC arises from mutations in the cells of hair follicles. Consequently, areas without hair follicles—such as the lips, palms, soles, and vulva minora—are unlikely to develop BCC.
Symptoms: BCC typically appears as a skin-coloured, pink, or pigmented nodule or plaque with a pearly edge and can ulcerate. Different types include nodular, superficial, morphoeic, and the more aggressive basosquamous carcinoma.


Treatment Necessity
Despite its low risk for metastasis, BCC requires treatment to prevent extensive local damage. If you have an upcoming holiday or important event. You can have up to 6 months to schedule your excision. Treatment options include –
- Surgical Excision: Often the first choice, providing clear margins to ensure complete removal.
- Mohs Surgery: Ideal for facial and other complex areas, preserving healthy tissue while thoroughly removing cancer cells. We will involve your care with a Dermatologist who specialises in Mohs Surgery.
- Less Invasive Treatments: Cryotherapy, photodynamic therapy, and topical treatments are options for less aggressive or superficial BCCs.
3. Squamous Cell Carcinoma (SCC)
Squamous Cell Carcinoma (SCC) is a type of skin cancer that can develop from precursors like actinic keratosis, a result of prolonged UV exposure. Without intervention, actinic keratosis can progress to intraepidermal carcinoma (IEC) and then to invasive SCC, which may penetrate deeper skin layers and potentially metastasise.
This progression highlights the importance of early detection and preventive treatment.


Preventative Treatment
Preventive measures are crucial in managing the risk of SCC. While acknowledging the benefits of Sunlight for vitamin D synthesis and mental health, it is essential to balance this with protective strategies to minimise sun damage.
The Importance of Early Treatment
Addressing skin changes promptly when they are less severe—not only saves skin but also lives. Treatments for early stages, like cryotherapy for actinic keratosis, topical medications for IEC, PDT field treatments are generally simple and highly effective. These early interventions prevent the progression to invasive SCC, thereby reducing the risk of metastasis and more complicated treatments required at later stages.
Long-Term Monitoring
Once treated for any stage of SCC progression, ongoing monitoring is essential. Regular follow-ups of 6monthly visits are recommended as this help catch any new changes early and maintain healthy skin over the long term.
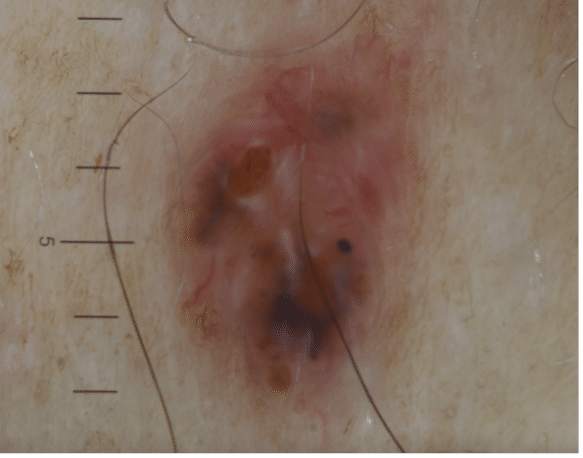
4. Melanoma
Understanding Melanoma: Australia’s National Cancer
Australia has the highest melanoma rates worldwide, often called ‘Australia’s national cancer.’ It’s crucial to recognise its prevalence and severity because of its potential for early detection and successful treatment. Melanoma can spread to many body parts, commonly affecting the lymph nodes, lungs, liver, bones, and brain. Early detection is key to managing its spread effectively.
Key Statistics
- Annual Diagnoses: Approximately 16,800 Australians are diagnosed each year.
- Mortality Rate: Around 1,300 Australians die annually from melanoma.
- Most common cancer in Australians aged 20 to 39.
- Second most common in men, after prostate cancer.
- Third most common in women, after breast and colorectal cancer.
Prevention and Detection
Early detection can lead to a 90% cure rate through surgical intervention.
Significant progress has been made in the last decade, with the 5-year survival rate for advanced melanoma increasing from less than 10% to over 50%.
How to Check Your Skin
ABCDE Method of Identifying Melanoma
A for Asymmetry: One half of the spot does not match the other.
B for Border: Edges are irregular, ragged, or blurred.
C for Colour: Varies within the same spot.
D for Diameter: Larger than 6mm or growing.
E for Evolving: Any change in size, shape, colour, or symptoms such as itching or bleeding.
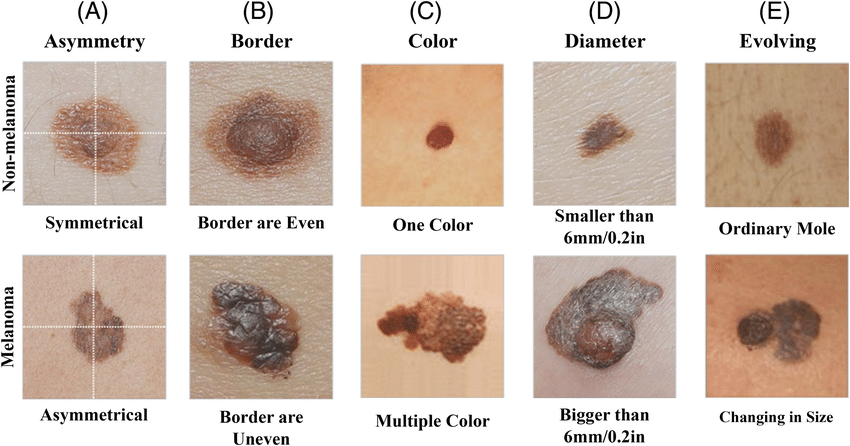 Image source: https://www.researchgate.net/figure/Illustration-of-ABCDE-criteria-for-skin-cancer-detection_fig2_359338536
Image source: https://www.researchgate.net/figure/Illustration-of-ABCDE-criteria-for-skin-cancer-detection_fig2_359338536
If you notice any changes or new spots on your skin, don’t hesitate to book a quick spot check. Dr. Tina Fang and Dr. Jack Fu are committed to addressing your concerns promptly. Even if you suspect it might be nothing, it’s always best to have it examined. At our clinic, we use Dermatoscopy to provide a thorough assessment, ensuring that even the smallest changes are carefully evaluated. It’s always better to be safe and have any changes checked by our experts.
Treatments Available
Discover our advanced and personalised treatment options for effectively managing and treating skin cancer.
Biopsies & Excisions
After your skin check, our doctors might recommend a biopsy if they spot a suspicious lesion.
This common procedure is performed under local anaesthesia right in your doctor’s room and involves removing a small sample of skin for laboratory analysis.
This detailed examination helps accurately diagnose any skin condition, guiding the next steps for your treatment.
Preparing for a skin excision involves several important steps:
Discussion and Health Review
Initially, our doctors will explain the procedure, including its purpose, potential risks, benefits, and costs. It’s important to provide a detailed medical history, including any allergies, medications, and existing health conditions.
Medication Adjustments
Some supplements or NSAIDS may need to be adjusted or stopped temporarily to avoid complications during surgery. However, it’s crucial not to stop any heart medications unless specifically instructed, as the risks from stopping these can outweigh the benefits.
Eating Before Surgery
Having a light meal a few hours before surgery can help maintain normal blood sugar levels. This is especially important because low blood sugar can cause feelings of nausea or faintness during a procedure.
Skin Preparation
The night before or the morning of the surgery, you should wash the area with mild soap and water to minimise the risk of infection. It’s also advisable to shave the area around the excision site if there is significant hair growth, as this can interfere with the procedure and dressing adhesion.
Assistance and Comfort
Arrange for someone to drive you home after the procedure, especially if you’re having surgery on an area that could impair your ability to drive or perform daily tasks. Wear loose, comfortable clothing that does not irritate the surgical site.
Day of Procedure
Arrive early to fill out paperwork and to discuss any last-minute questions or concerns with our doctors. This is also a good time to discuss any anxieties you might have so that they can be addressed before the procedure begins.
Proper aftercare is crucial to ensure successful healing and to prevent complications like infection or excessive scarring:
Keep the Wound Clean and Dry
24-48 hours for biopsies, and 5 days for excisions. It is important to keep the area clean and dry to aid the healing process.
Care for the Dressing
If the dressing becomes soaked with blood or other fluids, it should be changed to a clean and dry dressing.
Monitor for Infection
Watch for signs of infection, such as increased redness, swelling, warmth, pain, or discharge. If you notice any of these symptoms, contact our clinic immediately.
Book Now. No referrals required.
Our Skin Check, Cosmetic and Laser services are confidential, gentle and friendly to ensure patient comfort and safety throughout the whole process. Our experienced doctors will guide you and expert advice, so you can make confident and informed decisions.