What is Melanoma? Understanding This Aggressive Skin Cancer
Melanoma is the most dangerous form of skin cancer, arising from melanocytes—the cells responsible for producing melanin, the pigment that gives skin its colour. Although melanoma accounts for only a small percentage of skin cancer cases, it causes the majority of skin cancer-related deaths due to its high potential for metastasis.
Unlike basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), which typically remain localised, melanoma can spread rapidly to lymph nodes and internal organs if not detected early. While melanoma can develop anywhere on the body, it most commonly appears on the back, legs, arms, and face. In men, melanomas are more likely to develop on the trunk, whereas women often develop them on the legs.
There are several subtypes of melanoma, including:
- Superficial spreading melanoma – The most common type, which grows outward before penetrating deeper.
- Nodular melanoma – A fast-growing and aggressive form that quickly invades deeper skin layers.
- Lentigo maligna melanoma – Typically found in older adults, this type develops in sun-damaged skin and grows slowly.
- Acral lentiginous melanoma – A rare type that occurs on the palms, soles of the feet, and under the nails, more common in people with darker skin tones.
Melanoma is highly treatable when caught early, but delayed diagnosis significantly reduces survival rates.
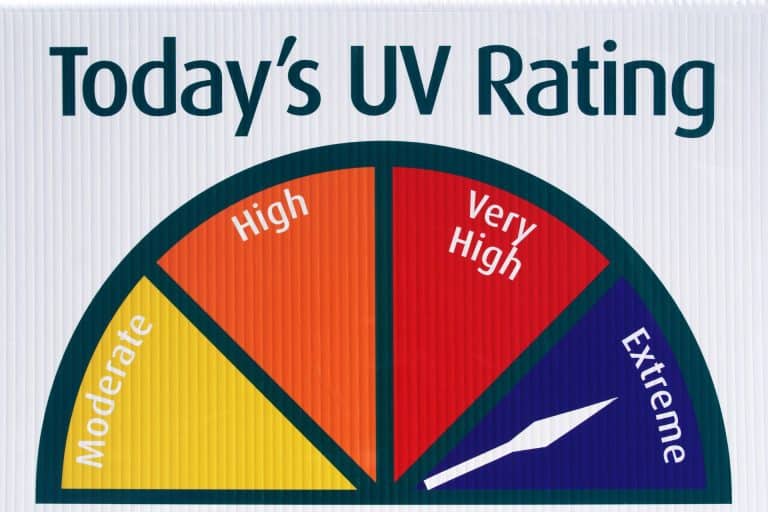
The Role of UV Exposure in Melanoma Development
Ultraviolet (UV) radiation from the sun or artificial sources, such as tanning beds, is the primary environmental risk factor for melanoma. UV exposure damages the DNA of skin cells, leading to mutations that can cause uncontrolled cell growth. While fair-skinned individuals are at the highest risk, anyone can develop melanoma.
Key Risk Factors:
- Intermittent, intense sun exposure – Sunburns, especially in childhood, significantly increase melanoma risk.
- Use of tanning beds – Artificial UV radiation from tanning beds is a well-established carcinogen.
- Fair skin, light hair, and blue or green eyes – Less melanin means reduced natural protection against UV damage.
- Family history of melanoma – Individuals with a first-degree relative diagnosed with melanoma have a higher genetic risk.
- Presence of many moles or atypical moles – A high number of moles, especially large or irregular ones, increases risk.
- Weakened immune system – People with immunosuppression, such as organ transplant recipients, are more susceptible to melanoma.
While UV exposure is the leading cause, melanoma can also develop in areas that receive little to no sunlight, indicating a role for genetic mutations beyond sun damage.

How to Identify the ABCDEs of Melanoma
Detecting melanoma early is critical, and the ABCDE rule provides a reliable guide for identifying suspicious moles or skin lesions:
- A – Asymmetry: One half of the mole does not match the other.
- B – Border: The edges are irregular, ragged, or poorly defined.
- C – Colour: Multiple colours or uneven pigmentation (brown, black, red, white, or blue).
- D – Diameter: Larger than 6mm (about the size of a pencil eraser).
- E – Evolving: Any change in size, shape, colour, or symptoms (itching, bleeding, or crusting) over time.
Additional Warning Signs:
- A new mole that appears suddenly in adulthood.
- A sore that does not heal or keeps recurring in the same spot.
- A lesion that becomes itchy, painful, or starts to bleed without provocation.
- Dark streaks under the nails, which could indicate subungual melanoma.
Regular self-examinations and professional skin checks are essential for early detection.
Treatment Options: Surgery, Immunotherapy, and Targeted Therapy
Melanoma treatment depends on the stage at diagnosis. Early-stage melanoma can often be cured with surgical excision, while advanced melanoma may require systemic treatments such as immunotherapy or targeted therapy.
1. Surgery
For localised melanoma, surgery is the primary treatment. The procedure involves:
- Wide local excision: The tumour and a margin of healthy tissue are removed.
- Sentinel lymph node biopsy (SLNB): If the tumour is deep, a biopsy is performed to check for cancer spread to nearby lymph nodes.
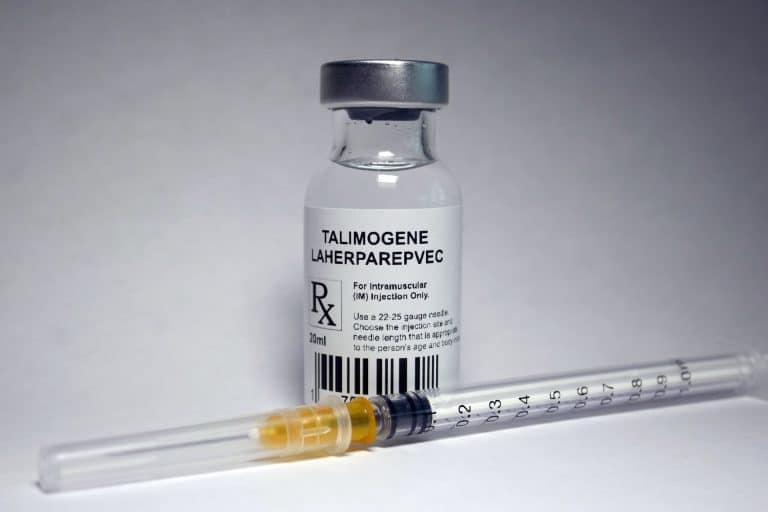
2. Immunotherapy
Immunotherapy helps stimulate the body’s immune system to attack melanoma cells. This treatment is particularly effective for advanced melanoma that has spread beyond the skin.
- Checkpoint inhibitors (e.g., pembrolizumab, nivolumab) block proteins that prevent the immune system from attacking cancer cells.
- Interleukin-2 therapy helps boost immune activity against melanoma but is used less frequently due to side effects.
3. Targeted Therapy
For melanomas with specific genetic mutations, targeted therapies can effectively block the growth of cancer cells.
- BRAF inhibitors (e.g., vemurafenib, dabrafenib) target the BRAF mutation present in about 50% of melanomas.
- MEK inhibitors (e.g., trametinib, cobimetinib) block pathways that help melanoma cells grow.
4. Radiation Therapy
Radiation therapy is sometimes used to manage metastatic melanoma or to treat melanoma that has spread to the brain.
5. Chemotherapy
Although less commonly used due to the success of immunotherapy and targeted therapy, chemotherapy may be an option for patients whose melanoma does not respond to other treatments.
Preventative Strategies for Reducing Melanoma Risk
1. Sun Protection
- Use sunscreen: Apply broad-spectrum SPF 30+ sunscreen daily, even on cloudy days.
- Wear protective clothing: Long-sleeved shirts, hats, and sunglasses provide added defence against UV exposure.
- Seek shade: Avoid direct sunlight during peak hours (10 a.m. – 4 p.m.).
- Avoid tanning beds: Artificial UV exposure significantly increases melanoma risk.
2. Regular Skin Checks
- Conduct monthly self-examinations, using mirrors to inspect hard-to-see areas.
- Visit a dermatologist annually, especially if you have a high-risk profile.
3. Know Your Risk Factors
- If you have many moles, a family history of melanoma, or fair skin, take extra precautions.
- Consider genetic counselling if multiple family members have had melanoma.
4. Vitamin D and Sun Safety
- Obtain vitamin D safely through diet and supplements rather than excessive sun exposure.
- Balancing sun exposure while preventing melanoma is essential for maintaining skin health.
Conclusion
Melanoma is an aggressive skin cancer that requires vigilance for early detection. Understanding the ABCDEs of melanoma, recognising risk factors, and adopting preventative measures can significantly reduce the likelihood of developing this disease.
Treatment options have advanced significantly, with surgery, immunotherapy, and targeted therapy offering promising outcomes, even for advanced cases. However, prevention remains the best strategy. By protecting the skin from UV radiation, performing regular skin checks, and seeking medical advice for suspicious lesions, individuals can greatly improve their chances of detecting melanoma early, when it is most treatable.
Public awareness, education, and early intervention are key to reducing the global burden of melanoma and improving survival rates.
Book a skin cancer check today at ISO Skin Cancer Clinic!